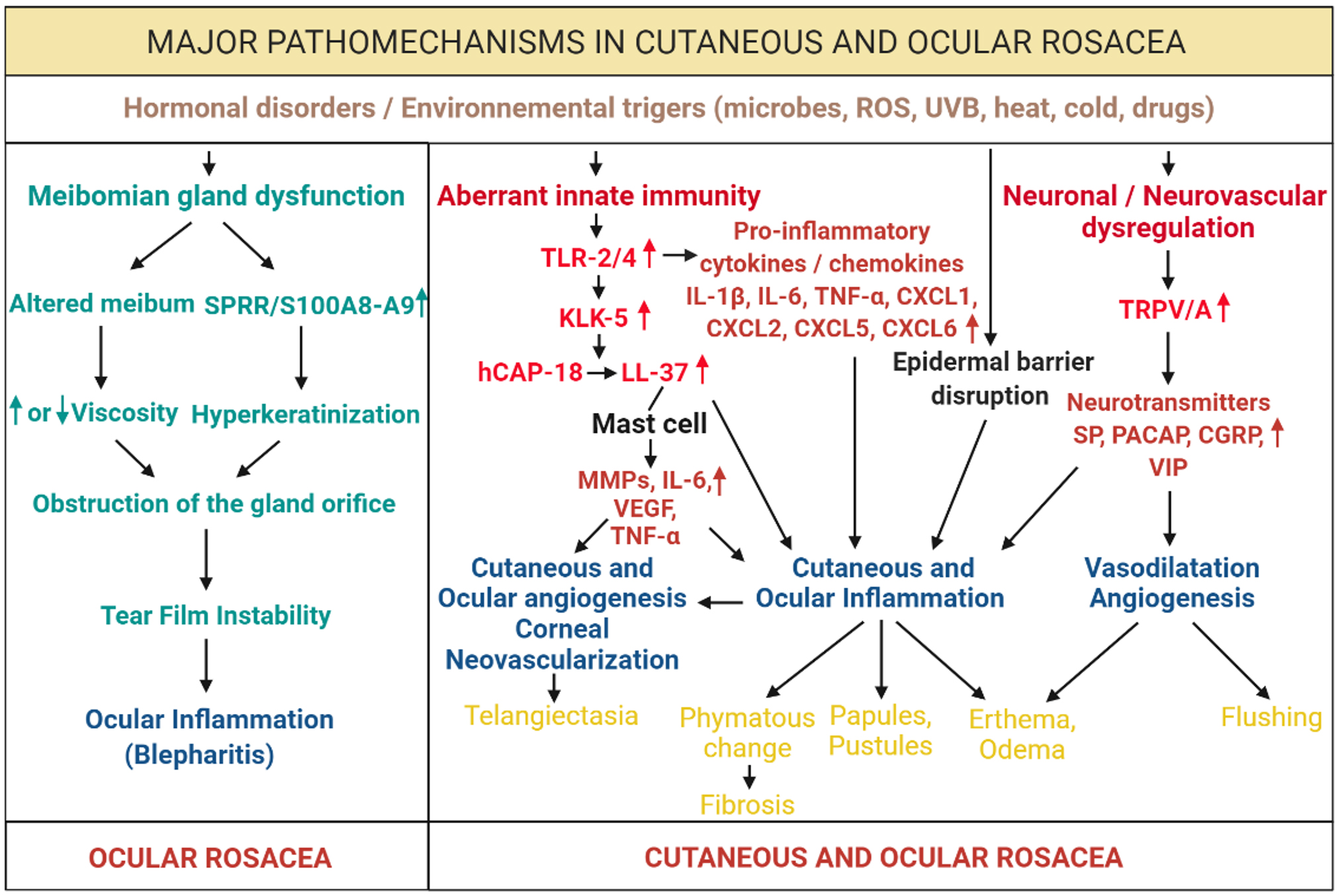
Figure 5. Major mechanisms of cutaneous and ocular rosacea. Excessive activation of innate immunity by various external and internal
stimuli, including hormonal dysfunctions, microbes, reactive oxygen species (ROS) or ultraviolet (UV) radiation, leads to
overexpression of Toll-like receptors (TLRs), including TLR-2 and 4. The release of proinflammatory cytokines, including interleukins
(ILs) and tumor necrosis factor-α (TNF-α), and chemokines, including chemokine (C-X-C motif) ligand (CXCL) 1, CXCL2, CXCL5,
and CXCL6, lead to inflammation and the development of papules, pustules, erythema, and edema. If the inflammation becomes
persistent, patients develop a phyma, leading to fibrosis. At the same time, TRL-2 and 4 upregulate kallikrein 5 (KLK-5),
which activates the cleavage of 18-kDa cationic antimicrobial protein (hCAP-18) into a biologically active peptide, LL-37.
LL-37 facilitates the degranulation of mast cells, which leads to a greater release of matrix metalloproteinases (MMPs), IL-6,
TNF-α, and the vascular endothelial growth factor (VEGF) participating in the cutaneous and ocular angiogenesis processes,
which can lead to corneal neovascularization and appearance of telangiectasias. Microorganisms, including Demodex, can also directly disrupt the epidermal barrier, which can lead to worsening of inflammation processes. Heat and cold and
environmental stimuli overactivate receptive potential channels transient receptor potential (TRP), including s), leading
to a significant release of neuropeptides, including substance P (SP), the pituitary adenylate cyclase-activating polypeptide
(PACAP), the peptide linked to the calcitonin gene (CGRP), and the vasoactive intestinal peptide (VIP), which cause neurovascular
dysfunction, leading to the processes of inflammation, vasodilation, and angiogenesis with the appearance of redness and worsening
of erythema and edema. Patients with ocular rosacea also have a dysfunction of the meibomian glands due to an alteration of
the meibum, compared with the sebum in patients with cutaneous rosacea. Overexpression of the genes coding for the small proline-rich
protein (SPRR) and calcium binding proteins (S100) A8 and A9 can lead to inflammation of the eyes and of the eyelid (blepharitis).
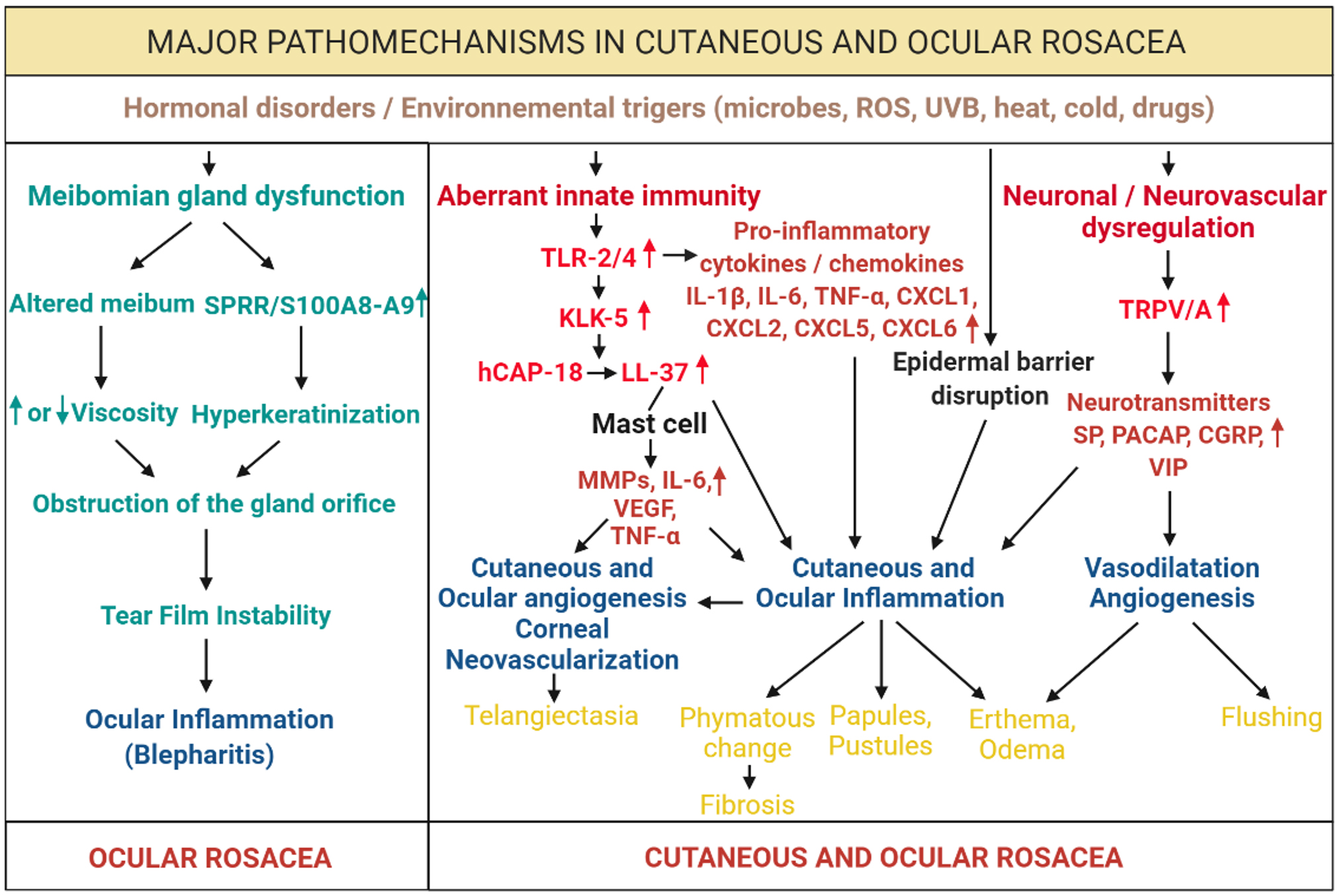
 Figure 5 of
Rodrigues-Braz, Mol Vis 2021; 27:323-353.
Figure 5 of
Rodrigues-Braz, Mol Vis 2021; 27:323-353.  Figure 5 of
Rodrigues-Braz, Mol Vis 2021; 27:323-353.
Figure 5 of
Rodrigues-Braz, Mol Vis 2021; 27:323-353.