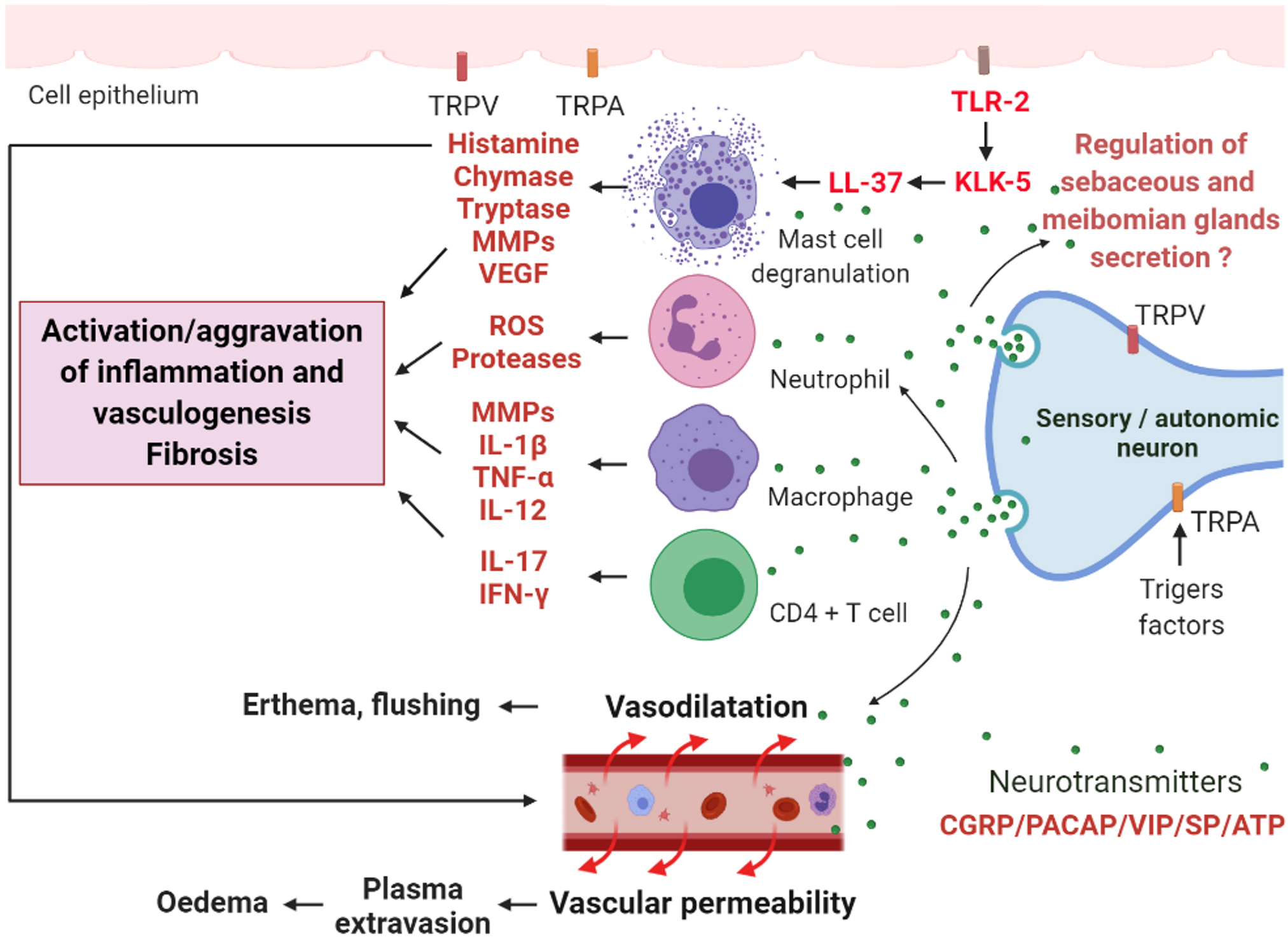
Figure 4. Possible mechanisms of neuronal and neurovascular deregulation in the rosacea pathophysiology mediated by the transient receptor
potential (TRP) channel family. Vanilloid TRP (TRPV) and ankyrin TRP (TRPA), among others, are expressed in neuronal and nonneuronal
cells and activated by external stimuli, such as heat, cold, or UV B (UVB) irradiation, and they are significantly regulated
upwards in rosacea. An influx of Ca2+ by the activation of these receptors induces the release of neuropeptides such as substance P (SP), the peptide related to
the calcitonin gene (CGRP), the polypeptide activator of the pituitary adenylates (PACAP), the intestinal vasoactive peptide
(VIP), and ATP. These neuropeptides can stimulate immune cells, such as mast cells, neutrophils, macrophages, and CD4+ T cells,
that release proinflammatory mediators, such as matrix metalloproteinases (MMPs), tumor necrosis factor-α (TNF-α), interferon-γ
(IFN-γ), interleukins (ILs), proteases, and reactive oxygen species (ROS), leading to the initiation or aggravation of inflammation.
Toll-like receptor 2 (TLR-2) activates kallikrein 5 (KLK-5), which activates the antimicrobial peptide of cathelicidin (LL-37).
LL-37 is known to be an activating factor of mast cells. Furthermore, mast cells can also release VEGF, contributing to vasculogenesis.
The action of neuropeptides on blood vessels leads to vasodilation, which is responsible for erythema and flushing, and to
vascular permeability, which is responsible for plasma extravasation, leading to edema. The release of histamine from mast
cells promotes vasodilation and the onset of fibrosis. The release of VEGF by mast cells promotes vasculogenesis. The sebaceous
and meibomian glands exhibit sensory and autonomic nerve regulation with the expression of neurotransmitters. This regulation
could contribute to the development of the disease.
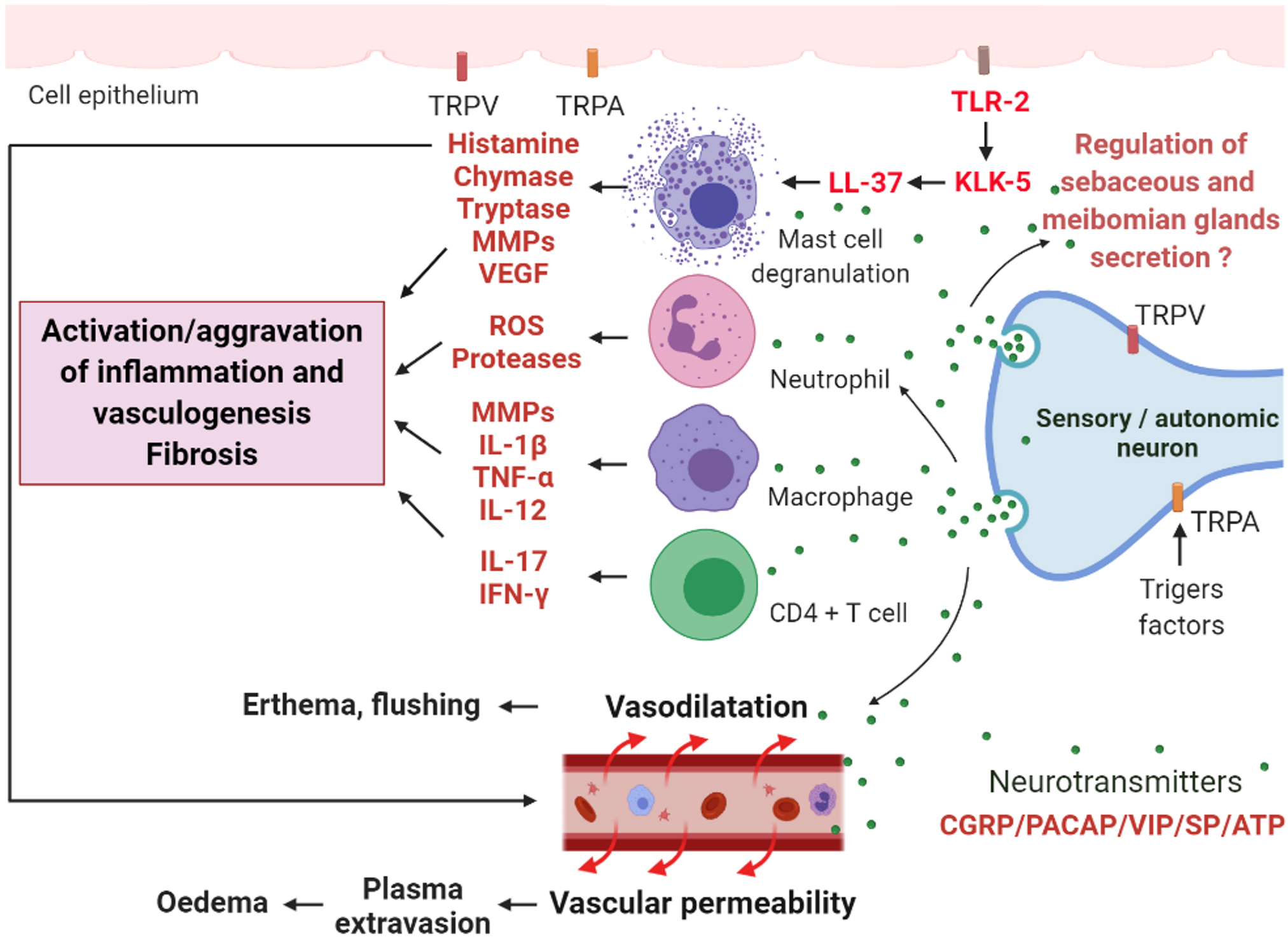
 Figure 4 of
Rodrigues-Braz, Mol Vis 2021; 27:323-353.
Figure 4 of
Rodrigues-Braz, Mol Vis 2021; 27:323-353.  Figure 4 of
Rodrigues-Braz, Mol Vis 2021; 27:323-353.
Figure 4 of
Rodrigues-Braz, Mol Vis 2021; 27:323-353.